INPatient
Residents rotate through inpatient services at North Shore University Hospital (NSUH) and Long Island Jewish Medical Center (LIJMC)—two hospitals that are geographically located only about one mile apart from one another but that expose residents to very unique patient populations and disease pathologies. After finishing training at our program, residents will be equipped to treat just about any patient or clinical condition. Inpatient rotations for residents include: general internal medicine teaching services, night float, the medical intensive care unit (MICU), the cardiac intensive care unit (CICU), an emergency medicine rotation, rotations for third-year residents as the medical admitting resident (MAR), and elective rotations. Residents provide care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Through practice based learning and improvement, residents build their medical knowledge base, demonstrate professionalism, gain skill in interpersonal communication, and learn to practice in the larger context and system of healthcare.
-

Ava-Dawn Gabbidon, MD
SITE DIRECTOR, LONG ISLAND JEWISH MEDICAL CENTER
-

Jared Honigman, DO
SITE DIRECTOR, NORTH SHORE UNIVERSITY HOSPITAL
-
Eileen Kim, MD
ASSOCIATE PROGRAM DIRECTOR, NORTH SHORE UNIVERSITY HOSPITAL
-

Edward Vuong, MD
ASSOCIATE PROGRAM DIRECTOR, LONG ISLAND JEWISH MEDICAL CENTER
Inpatient sites
North Shore university hospital
A quaternary care center that is located in Manhasset, NY and is the center of cardiac, pulmonary, renal, and hepatic transplantation services for all of Northwell Health.
Long island jewish medical center
A quaternary care center that is located in New Hyde Park, NY and is home to Northwell Health’s advanced lung disease and veno-venous extracorporeal membrane oxygenation (ECMO) program and is located directly across the street from the Zuckerberg Cancer Center.
inpatient medicine
Residents rotate through inpatient medicine at NSUH and LIJMC and learn to evaluate and mange any patient suffering from any pathology.
Each team is on call every fourth day until 7 pm when sign out to the night float is scheduled. Medical students (mostly from the Zucker School of Medicine at Hofstra/Northwell but also from Albert Einstein College of Medicine and SUNY Downstate) and, at times, pharmacists, podiatry residents, oral and maxillofacial surgery residents, or psychiatry residents will be a part of the team.
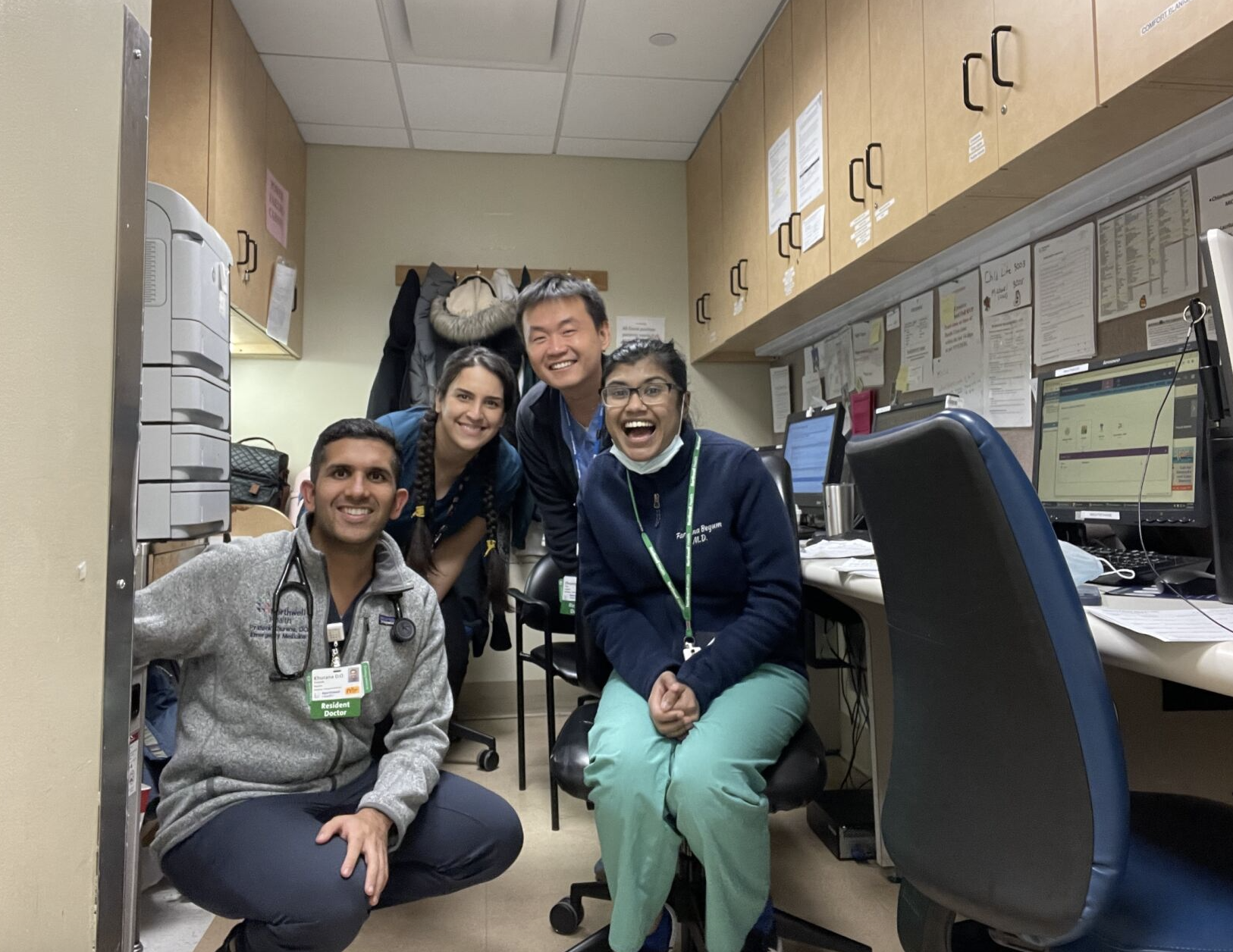
To the right, Kishen Bulsara, MD takes us through a day in the life on floors as an intern:

medical ICU
At NSUH and LIJMC, residents rotate in some of the premier medical intensive care units in the world. Under the direct supervision of expert attending physicians, and fellows, in pulmonary and critical care medicine, residents manage patients who suffer from shock (in all forms), acute and chronic lung injury, acute and chronic renal failure, infections, encephalopathy, and more. Residents gain experience managing patients who require vasopressors, sedatives, invasive mechanical ventilation, and, in some cases, end-of-life care. Our fellows and faculty have particular expertise in point-of-care ultrasound (POCUS). Every year, they lead educational sessions at national and international conferences, and residents learn from them daily.

Cardiac ICU
Residents rotate through the cardiac intensive care units at NSUH and LIJMC. They gain experience managing patients who suffer from cardiogenic shock, arrhythmias, acute myocardial infarctions, and pericardial diseases. In addition to their cardiac conditions, these patients often have several medical comorbidities. Residents gain experience interpreting readings from swan-ganz catheters and managing patients who require trans-venous pacing or mechanical circulatory support through intra-aortic balloon pumps or Impella devices. They also have exposure to patient telemetry readings and advanced cardiac imaging modalities—such as trans-thoracic and trans-esophageal echocardiography, cardiac MR, and cardiac CT. Residents evaluate and manage patients under the direct supervision of expert attending physicians—many of whom are board certified in both cardiology and critical care medicine—and cardiology fellows. The director of the CICU, Dr. Matthew Pierce, is frequently voted by the residents as a teacher of the year.

Elective rotations
Residents assigned to elective rotations participate in the inpatient and outpatient activities of that service. In general residents work 8am-5pm Mondays through Fridays. Elective opportunities exist in all subspecialties of internal medicine. Any electives outside of the department of medicine require the approval of the program director and a written curriculum.
A Night as an intern
By Shreya Srivastava, MD, MPH
Night float consists of two interns each night who are responsible for all the house staff patients (about 50 patients per intern). Although tiring and unpredictable, night float is one of the key rotations to developing an appropriate level of independence and confidence as a new doctor.
6:30pm-7pm
I receive a detailed sign out from four house staff teams with the patients I will be covering overnight, including follow-up tasks. I make sure to ask for any contingency plans—a good sign out will make the night go smoother! I listen extra carefully for the “watcher” patients who are high risk for decompensation.
7pm-7:30pm
I generate a schedule for the night by creating a collated to-do list organized by hour of the night. This helps me ensure I don’t miss any tasks the day team requested.
7:30pm–8pm
Time permitting, I’ll go and assess the “watcher” patients. This gives me an idea of how they appear when they are stable so that if they do decompensate, I will be able to easily identify changes.
8pm-12am
Each night, I admit one new patient to the medicine service. After reviewing the chart, obtaining the history and physical and developing a plan for the patient, I discuss the patient’s case with a hospitalist attending.
Throughout the night
As the night float intern, I am required to employ independent decision making to address acute issues that occur overnight with my patients. If I have any questions, the MAR is always willing to help. Night float is also a great time to practice procedures such as arterial sticks and ultrasound guided IVs.
At any point in the night, if there is a rapid response called, we attend to these patients. The MAR runs these rapids, however, sometimes there are several simultaneously and as an intern I have to rise to the occasion and become the leader. While this may sound scary, there is plenty of support between nursing staff, clinical impact team responders and the respiratory team. In rapids, it is especially important to gather the input and utilize the knowledge of the multidisciplinary team as this helps me develop a plan in the acute setting.
6:30am–7am
The sun is shining and it’s time to sign out to the day team regarding the overnight events. Afterwards, I head home to relax, draw my blackout curtains, and rest up for the next night!